You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
NHS hospital waiting lists
- Thread starter bear66
- Start date
Ingleby_Flash
Well-known member
When they scrapped the targets for waiting times it was obvious which way it was going. Soon be bad enough to justify flogging it off to some American corp.
Cut costs 5% year on year and all that is left to save on is staff.
Not enough staff you can't provide a robust safe service.
Only so many frontline efficiency savings to be made in quality improvement.
Covid led to money being thrown at the NHS but after the horse had bolted.
Vaccinations is a perfect example. Amazing service set up across the UK. But very few of the staff supporting it are new to the NHS, they are all redeployed from other services leaving them short and adding to waiting lists or absences of service/ care.
Not enough staff you can't provide a robust safe service.
Only so many frontline efficiency savings to be made in quality improvement.
Covid led to money being thrown at the NHS but after the horse had bolted.
Vaccinations is a perfect example. Amazing service set up across the UK. But very few of the staff supporting it are new to the NHS, they are all redeployed from other services leaving them short and adding to waiting lists or absences of service/ care.
Jonny_Rondos_Disco_pants
Well-known member
In good news, my dad finally managed to get a consultation 2.5 months ago for a knee replacement after everything was cancelled last year. They had him in 2 weeks ago.
Certain things they are working their way through the lists. Ging to be some battle to get on top of it
Certain things they are working their way through the lists. Ging to be some battle to get on top of it
Archiestephens_elbow
Well-known member
Because Diane abbot had a can of mojito on a train and miliband dropped a bacon sandwich
Sheriff_John_Bunnell_ret
Well-known member
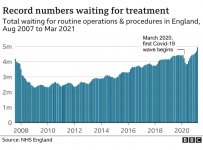
Note the drop just when covid kicks in.
Is this a change in the way "being on the waiting list" is counted, or is it covid killing a bunch of vulnerable people?
Is this a change in the way "being on the waiting list" is counted, or is it covid killing a bunch of vulnerable people?
Blf
Well-known member
A young member of our family has been struggling with school and life in general. We have been very concerned for him and sought help via his GP. He was referred to CAMH's for assessment/treatment . We got a letter saying he would be seen but there is a two year waiting list 
Randy
Well-known member
If the parents can afford mate if seriously consider getting some private help for him.A young member of our family has been struggling with school and life in general. We have been very concerned for him and sought help via his GP. He was referred to CAMH's for assessment/treatment . We got a letter saying he would be seen but there is a two year waiting list
S7DiscoDown
Well-known member
Dentists are every bit as bad. Unless you go private and pay and suddenly a place 'opens up' 
I know we had waiting lists in the NHS before covid but I'm sure it's a pretty valid excuse now? They simply haven't been seeing anyone for minor surgery etc.
I know we had waiting lists in the NHS before covid but I'm sure it's a pretty valid excuse now? They simply haven't been seeing anyone for minor surgery etc.
Corcaigh_the_Cat
Well-known member
I think it may depend on how well manned particular departments are. I've had 5 bouts of surgery in the past year, 3 plastic surgery and 2 eye ops.
That could also be related to me having regular follow up appointments?
All off my ops were under local anaesthetic on a day visit basis.
The theatres are busy, my NHS ops were carried out at JCUH, Redcar PCT and the Nuffield in Norton.
That could also be related to me having regular follow up appointments?
All off my ops were under local anaesthetic on a day visit basis.
The theatres are busy, my NHS ops were carried out at JCUH, Redcar PCT and the Nuffield in Norton.
Corcaigh_the_Cat
Well-known member
Dentists are every bit as bad. Unless you go private and pay and suddenly a place 'opens up'
I know we had waiting lists in the NHS before covid but I'm sure it's a pretty valid excuse now? They simply haven't been seeing anyone for minor surgery etc.
That last bit isn't true, surgery is going ahead, including minor surgery.
Oh, and I've received emails from my dentist asking me to go for the check up I missed.
Don't believe all of the gossip.
Nobby_Barnes
Well-known member
I know Middlesbrough Mind have a young people's/schools project. Try there if your family member is localA young member of our family has been struggling with school and life in general. We have been very concerned for him and sought help via his GP. He was referred to CAMH's for assessment/treatment . We got a letter saying he would be seen but there is a two year waiting list
Malaguena
Well-known member
There was an interesting article by Dr Mark Porter in The Times this morning. Behind a paywall so copied here ...
I am writing this on a glorious bank holiday morning but, as ever, the day job is on my mind and I can see dark clouds on the horizon. Even assuming that the worst of the pandemic is over here in the UK — and that is an optimistic assumption — the backlog it has created in the NHS looms large. Or, to put it another way, even if we master Covid it could take the rest of my working life* to reverse its legacy. So how is this going to affect you, and what can you do about it?
The pandemic may be bearing the brunt of the blame, but in truth the NHS was struggling to cope long before it started. Thanks to a significant boost in funding waiting times fell to a low in 2010, but by 2014 the trend was reversing. And in the months before Covid hit there were already nearly four and a half million people on waiting lists in England. The pandemic may have added another half million but in reality it’s just the final straw for a system that was already creaking. The NHS couldn’t meet demand when it was working at 100 per cent capacity pre-Covid and, thanks to continuing restrictions, it is now still only functioning at about 80 per cent capacity. The knock-on effects are plain to see.
Delays in cancer therapy may grab the headlines, but every part of the system is affected, from people waiting for a new hip or knee to children with tooth decay. And it is not just operating theatres and outpatient clinics, but every part of the patient pathway, from imaging — such as CT scans — to pathology labs interpreting biopsy results.
If the NHS is to get rid of the backlog and return to 2019 waiting times (which were already too long) it is going to have to work at more than 100 per cent capacity, but how? Many of the staff are exhausted and demoralised (not least nurses, many of whom would swap a clap for an extra 1 per cent on their pay rise), and hospitals are struggling to recruit enough people to meet present demand, let alone staff clinics and theatres working overtime.
However, this is the NHS’s problem, not yours (unless you are unwell), and we are going to have to deal with it. I only hope our masters realise the scale of the problem.
If you are unfortunate enough to need some form of hospital care over the next few years, then I am afraid your patience is likely to be tested, but there are steps you can take to help.
First, be flexible and be prepared to travel. For example, my local hospitals in Gloucestershire have just announced they are not accepting any new referrals for people with hernias because they have such a huge backlog. However, independent providers (private or charitable hospitals contracted to the NHS) in the county, and across the border in Wiltshire, are still accepting patients and able to offer surgery within 8 to 12 weeks.
Don’t procrastinate. Many patients with arthritic hips and knees wait until they really can’t cope any more before opting to see a specialist but, given that you are likely to be waiting a year or more, it pays not to leave it too late. The time to talk to your GP is when you are starting to struggle, rather than when you are at the end of your tether.
Use the delay to your advantage. The outcomes for most surgery, whether it be to remove a cancerous lump or replace an arthritic joint, are improved if you are better prepared. Prehabilitation — where patients prepare for surgery by losing weight, getting fitter and stronger, stopping smoking and eating more healthily etc — is fast becoming routine in many hospitals and prolonged delays mean you really have no excuse. It makes the surgeon’s job easier, and is likely to give you a smoother and faster recovery, as well as a better result.
Alternatively you could try the private sector, which is, on the whole, nearly back at full speed after a very disruptive year (not least because many hospitals were seconded to the NHS to help during the worst of the pandemic). But unless you are insured the costs can be eye-watering (eg £2,000-3,000 for a hernia, £10,000-15,000 for a joint replacement). And seeing a specialist privately won’t mean you can jump the NHS queue (exceptions may be made if an urgent problem is discovered).
I normally try to end this column on a bright note, but this week I am going to be candid. The next few years are going to be tough — on NHS staff and patients — and the only silver lining I can see is that we are in this together, and no nation is better at queueing.
* About five years. I hit 60 next year, hopefully.
Patient patients
● There are nearly five million people on waiting lists for NHS hospital treatment in England alone — the highest number since records began in 2007.
● Just under one in ten of these have been waiting more than a year often for elective surgical procedures, such as hip and knee replacement. A million people have been waiting more than six months.
● As of February 2021 only two thirds of patients had been treated within the 18-week wait allowed (the target is 92 per cent).
● The NHS has not hit the 18-week target for five years.
● Waits vary in other parts of the UK but follow a similar pattern to England.
Source: the Royal College of Surgeons of England, rcseng.ac.uk
I am writing this on a glorious bank holiday morning but, as ever, the day job is on my mind and I can see dark clouds on the horizon. Even assuming that the worst of the pandemic is over here in the UK — and that is an optimistic assumption — the backlog it has created in the NHS looms large. Or, to put it another way, even if we master Covid it could take the rest of my working life* to reverse its legacy. So how is this going to affect you, and what can you do about it?
The pandemic may be bearing the brunt of the blame, but in truth the NHS was struggling to cope long before it started. Thanks to a significant boost in funding waiting times fell to a low in 2010, but by 2014 the trend was reversing. And in the months before Covid hit there were already nearly four and a half million people on waiting lists in England. The pandemic may have added another half million but in reality it’s just the final straw for a system that was already creaking. The NHS couldn’t meet demand when it was working at 100 per cent capacity pre-Covid and, thanks to continuing restrictions, it is now still only functioning at about 80 per cent capacity. The knock-on effects are plain to see.
Delays in cancer therapy may grab the headlines, but every part of the system is affected, from people waiting for a new hip or knee to children with tooth decay. And it is not just operating theatres and outpatient clinics, but every part of the patient pathway, from imaging — such as CT scans — to pathology labs interpreting biopsy results.
If the NHS is to get rid of the backlog and return to 2019 waiting times (which were already too long) it is going to have to work at more than 100 per cent capacity, but how? Many of the staff are exhausted and demoralised (not least nurses, many of whom would swap a clap for an extra 1 per cent on their pay rise), and hospitals are struggling to recruit enough people to meet present demand, let alone staff clinics and theatres working overtime.
However, this is the NHS’s problem, not yours (unless you are unwell), and we are going to have to deal with it. I only hope our masters realise the scale of the problem.
If you are unfortunate enough to need some form of hospital care over the next few years, then I am afraid your patience is likely to be tested, but there are steps you can take to help.
First, be flexible and be prepared to travel. For example, my local hospitals in Gloucestershire have just announced they are not accepting any new referrals for people with hernias because they have such a huge backlog. However, independent providers (private or charitable hospitals contracted to the NHS) in the county, and across the border in Wiltshire, are still accepting patients and able to offer surgery within 8 to 12 weeks.
Don’t procrastinate. Many patients with arthritic hips and knees wait until they really can’t cope any more before opting to see a specialist but, given that you are likely to be waiting a year or more, it pays not to leave it too late. The time to talk to your GP is when you are starting to struggle, rather than when you are at the end of your tether.
Use the delay to your advantage. The outcomes for most surgery, whether it be to remove a cancerous lump or replace an arthritic joint, are improved if you are better prepared. Prehabilitation — where patients prepare for surgery by losing weight, getting fitter and stronger, stopping smoking and eating more healthily etc — is fast becoming routine in many hospitals and prolonged delays mean you really have no excuse. It makes the surgeon’s job easier, and is likely to give you a smoother and faster recovery, as well as a better result.
Alternatively you could try the private sector, which is, on the whole, nearly back at full speed after a very disruptive year (not least because many hospitals were seconded to the NHS to help during the worst of the pandemic). But unless you are insured the costs can be eye-watering (eg £2,000-3,000 for a hernia, £10,000-15,000 for a joint replacement). And seeing a specialist privately won’t mean you can jump the NHS queue (exceptions may be made if an urgent problem is discovered).
I normally try to end this column on a bright note, but this week I am going to be candid. The next few years are going to be tough — on NHS staff and patients — and the only silver lining I can see is that we are in this together, and no nation is better at queueing.
* About five years. I hit 60 next year, hopefully.
Patient patients
● There are nearly five million people on waiting lists for NHS hospital treatment in England alone — the highest number since records began in 2007.
● Just under one in ten of these have been waiting more than a year often for elective surgical procedures, such as hip and knee replacement. A million people have been waiting more than six months.
● As of February 2021 only two thirds of patients had been treated within the 18-week wait allowed (the target is 92 per cent).
● The NHS has not hit the 18-week target for five years.
● Waits vary in other parts of the UK but follow a similar pattern to England.
Source: the Royal College of Surgeons of England, rcseng.ac.uk
bear66
Well-known member
And Hancock in charge to sort it out! At least we'll have"record" amounts going to the NHS.There was an interesting article by Dr Mark Porter in The Times this morning. Behind a paywall so copied here ...
I am writing this on a glorious bank holiday morning but, as ever, the day job is on my mind and I can see dark clouds on the horizon. Even assuming that the worst of the pandemic is over here in the UK — and that is an optimistic assumption — the backlog it has created in the NHS looms large. Or, to put it another way, even if we master Covid it could take the rest of my working life* to reverse its legacy. So how is this going to affect you, and what can you do about it?
The pandemic may be bearing the brunt of the blame, but in truth the NHS was struggling to cope long before it started. Thanks to a significant boost in funding waiting times fell to a low in 2010, but by 2014 the trend was reversing. And in the months before Covid hit there were already nearly four and a half million people on waiting lists in England. The pandemic may have added another half million but in reality it’s just the final straw for a system that was already creaking. The NHS couldn’t meet demand when it was working at 100 per cent capacity pre-Covid and, thanks to continuing restrictions, it is now still only functioning at about 80 per cent capacity. The knock-on effects are plain to see.
Delays in cancer therapy may grab the headlines, but every part of the system is affected, from people waiting for a new hip or knee to children with tooth decay. And it is not just operating theatres and outpatient clinics, but every part of the patient pathway, from imaging — such as CT scans — to pathology labs interpreting biopsy results.
If the NHS is to get rid of the backlog and return to 2019 waiting times (which were already too long) it is going to have to work at more than 100 per cent capacity, but how? Many of the staff are exhausted and demoralised (not least nurses, many of whom would swap a clap for an extra 1 per cent on their pay rise), and hospitals are struggling to recruit enough people to meet present demand, let alone staff clinics and theatres working overtime.
However, this is the NHS’s problem, not yours (unless you are unwell), and we are going to have to deal with it. I only hope our masters realise the scale of the problem.
If you are unfortunate enough to need some form of hospital care over the next few years, then I am afraid your patience is likely to be tested, but there are steps you can take to help.
First, be flexible and be prepared to travel. For example, my local hospitals in Gloucestershire have just announced they are not accepting any new referrals for people with hernias because they have such a huge backlog. However, independent providers (private or charitable hospitals contracted to the NHS) in the county, and across the border in Wiltshire, are still accepting patients and able to offer surgery within 8 to 12 weeks.
Don’t procrastinate. Many patients with arthritic hips and knees wait until they really can’t cope any more before opting to see a specialist but, given that you are likely to be waiting a year or more, it pays not to leave it too late. The time to talk to your GP is when you are starting to struggle, rather than when you are at the end of your tether.
Use the delay to your advantage. The outcomes for most surgery, whether it be to remove a cancerous lump or replace an arthritic joint, are improved if you are better prepared. Prehabilitation — where patients prepare for surgery by losing weight, getting fitter and stronger, stopping smoking and eating more healthily etc — is fast becoming routine in many hospitals and prolonged delays mean you really have no excuse. It makes the surgeon’s job easier, and is likely to give you a smoother and faster recovery, as well as a better result.
Alternatively you could try the private sector, which is, on the whole, nearly back at full speed after a very disruptive year (not least because many hospitals were seconded to the NHS to help during the worst of the pandemic). But unless you are insured the costs can be eye-watering (eg £2,000-3,000 for a hernia, £10,000-15,000 for a joint replacement). And seeing a specialist privately won’t mean you can jump the NHS queue (exceptions may be made if an urgent problem is discovered).
I normally try to end this column on a bright note, but this week I am going to be candid. The next few years are going to be tough — on NHS staff and patients — and the only silver lining I can see is that we are in this together, and no nation is better at queueing.
* About five years. I hit 60 next year, hopefully.
Patient patients
● There are nearly five million people on waiting lists for NHS hospital treatment in England alone — the highest number since records began in 2007.
● Just under one in ten of these have been waiting more than a year often for elective surgical procedures, such as hip and knee replacement. A million people have been waiting more than six months.
● As of February 2021 only two thirds of patients had been treated within the 18-week wait allowed (the target is 92 per cent).
● The NHS has not hit the 18-week target for five years.
● Waits vary in other parts of the UK but follow a similar pattern to England.
Source: the Royal College of Surgeons of England, rcseng.ac.uk